
Table of Contents
Section 1: Understanding Diabetes
1.1: What is Diabetes?
- Definition: Diabetes is a chronic condition that affects the body’s ability to process blood sugar, leading to elevated glucose levels. It can be caused by insufficient insulin production or the body’s inability to use insulin effectively.
- Types of Diabetes: There are different types of diabetes, including Type 1, Type 2, and gestational diabetes, each with distinct causes and characteristics.
- Risk Factors: Factors such as genetics, obesity, and sedentary lifestyle contribute to the development of diabetes, making it a prevalent health concern globally.
1.2: Symptoms and Diagnosis
- Common Symptoms: Symptoms of diabetes include increased thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision.
- Diagnostic Tests: Diagnosis involves blood tests to measure glucose levels, as well as additional tests to differentiate between Type 1 and Type 2 diabetes.
- Prevalence: Diabetes is a widespread condition, affecting millions of individuals worldwide, with a significant impact on public health.
1.3: Causes and Risk Factors
- Insulin Production: In Type 1 diabetes, the immune system attacks and destroys insulin-producing cells in the pancreas, leading to a lack of insulin. In Type 2 diabetes, the body becomes resistant to insulin or doesn’t produce enough.
- Genetic Predisposition: Family history and genetic factors play a role in the development of diabetes, increasing the risk for individuals with a family history of the condition.
- Lifestyle Influence: Sedentary lifestyle, poor dietary habits, and obesity are significant risk factors for the onset of Type 2 diabetes, highlighting the importance of lifestyle modifications.
1.4: Impact on Health
- Complications: Diabetes can lead to various health complications, including cardiovascular disease, kidney damage, nerve damage, and vision problems.
- Public Health Burden: The prevalence of diabetes poses a significant burden on healthcare systems, with implications for healthcare costs and resources.
- Global Perspective: Diabetes is a global health concern, affecting diverse populations and necessitating comprehensive strategies for prevention and management.
Section 2: Effects of Diabetes

2.1: Health Implications
- Cardiovascular Health: Diabetes is a major risk factor for cardiovascular diseases, including heart attacks, strokes, and peripheral vascular disease.
- Renal Function: The impact of diabetes on kidney function can lead to chronic kidney disease and necessitate dialysis or kidney transplantation.
- Neuropathy: Nerve damage due to diabetes can result in peripheral neuropathy, causing pain, tingling, and numbness in the extremities.
2.2: Vision and Foot Complications
- Vision Impairment: Diabetes can lead to diabetic retinopathy, a condition that affects the eyes and can cause blindness if left untreated.
- Foot Problems: Individuals with diabetes are prone to foot complications, including neuropathy-related ulcers and infections, which can lead to serious complications and amputations.
- Wound Healing: Impaired wound healing is a common issue for individuals with diabetes, leading to chronic wounds and an increased risk of infections.
2.3: Psychological Impact
- Emotional Well-being: Managing diabetes can have a significant impact on emotional health, leading to stress, anxiety, and depression.
- Quality of Life: The daily management of diabetes, including dietary restrictions and medication regimens, can affect the overall quality of life for individuals with the condition.
- Support Systems: Building strong support systems and access to mental health resources are crucial for addressing the psychological impact of diabetes.
2.4: Societal and Economic Effects
- Workplace Productivity: Diabetes can affect workplace productivity due to health-related absences and reduced work efficiency.
- Healthcare Expenditure: The economic burden of diabetes includes direct medical costs, as well as indirect costs related to productivity loss and disability.
- Social Stigma: Individuals with diabetes may face social stigma and discrimination, highlighting the need for awareness and advocacy to combat misconceptions.
Section 3: Managing Diabetes
3.1: Lifestyle Modifications
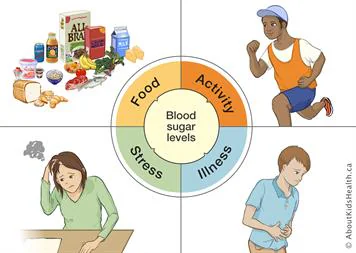
- Dietary Guidelines: A balanced diet with a focus on portion control, reduced sugar intake, and healthy food choices is essential for managing diabetes.
- Physical Activity: Regular exercise and physical activity play a crucial role in managing blood sugar levels and improving overall health.
- Stress Management: Stress reduction techniques, such as meditation and mindfulness, can contribute to better diabetes management.
3.2: Medication and Monitoring
- Insulin Therapy: For individuals with Type 1 diabetes or advanced Type 2 diabetes, insulin therapy may be necessary to regulate blood sugar levels.
- Oral Medications: Various oral medications are available to help manage blood glucose levels and improve insulin sensitivity.
- Blood Glucose Monitoring: Regular monitoring of blood sugar levels through self-testing is essential for adjusting treatment plans and maintaining control.
3.3: Patient Education and Support
- Self-care Skills: Patient education programs focus on empowering individuals with diabetes to develop self-care skills, including meal planning, medication management, and symptom recognition.
- Support Networks: Access to support groups, peer networks, and educational resources can provide valuable emotional and practical support for individuals with diabetes.
- Health Literacy: Enhancing health literacy and promoting awareness about diabetes management is critical for improving outcomes and reducing complications.
3.4: Preventive Strategies
- Early Detection: Screening and early detection programs can help identify individuals at risk for diabetes and initiate preventive interventions.
- Community Engagement: Community-based initiatives, including awareness campaigns and lifestyle programs, contribute to preventive strategies and promote healthy living.
- Policy Advocacy: Advocacy for policies supporting diabetes prevention, access to care, and research funding is essential for addressing the broader public health impact of diabetes.






